Patient Safety
What is Patient Safety?
“The simplest definition of patient safety is the prevention of errors and adverse effects to patients associated with health care. While health care has become more effective, it has also become more complex, with greater use of new technologies, medicines and treatments. Health services treat older and sicker patients who often present with significant co-morbidities requiring more and more difficult decisions as to health care priorities. Increasing economic pressure on health systems often leads to overloaded health care environments.” (World Health Organisation, 2017)
We aim to provide clinicians with the necessary information and resources in order to gain a better understanding of the concept of patient safety and to enable them to mitigate patient safety incidents within their own practise and clinical teams.
Is Patient Safety an Issue in Oral Surgery?
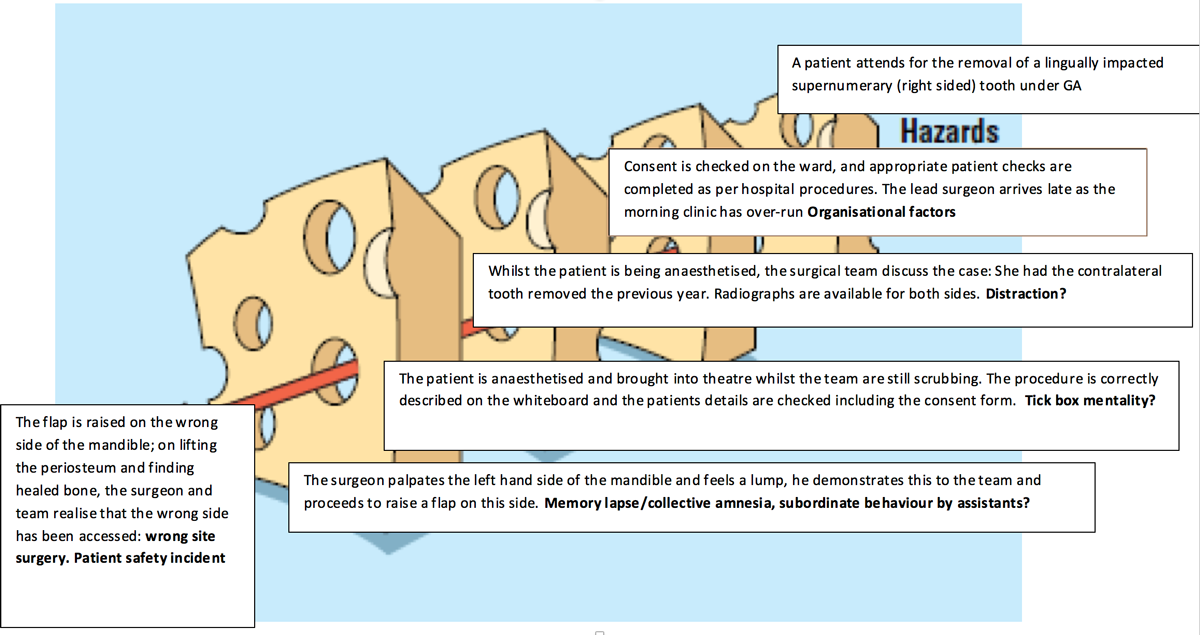
Yes, as Oral Surgeons, we perform a high volume of multi-site complex procedures on anxious patients who are frequently conscious that have the potential for error to occur; these errors are more likely to occur due to the number of teeth and contra laterality, including issues with charting and supernumerary or impacted teeth.
These errors or Patient Safety Incidents (PSIs) may be due to one or more of the following:
Human Factors
Human factors refer to environmental, organisational and job factors, and human and individual characteristics which influence behaviour at work in a way which can affect health and safety. A simple way to view human factors is to think about three aspects: the job, the individual and the organisation and how they impact on people’s health and safety-related behaviour
Systems Failures
Working with systems that are designed to provide safe care will help to reduce the incidence of adverse events in healthcare. Reducing error through systems changes include:
- Reducing complexity
- Optimising information processing
- Automating wisely
- Mitigating the unwanted effects of change
Patient Factors
Patients are increasingly encouraged to take an active role in their own healthcare.
Patients can act as ‘safety buffers’, but the responsibility for patient safety still lies with the clinician.
An example of these factors leading to a PSI is shown below:
Never Events
Between April 2015 and April 2021, extraction of the wrong tooth was included on the Never Events framework published by NHS England and NHS Improvement. It was announced in February 2021 that this was going to be removed from the framework due to a realisation that it did not fit the definition for a surgical never event.
Never events are defined as incidents with “the potential to cause serious patient harm or death” that are “wholly preventable where guidance or safety recommendations that provide strong systemic protective barriers are available at a national level and have been implemented by healthcare providers”.
Removal of the wrong tooth is still considered to be a serious incident and must be reported and investigated appropriately.
Patient Safety in Dentistry
A recent study found that the following events may be considered as adverse or never events related to dentistry (listed in order of risk to patient):
- Failure to check past medical history
- Inhalation or swallowing of a crown or instrument
- Restoring the wrong tooth
- Oxygen and/or emergency drugs not being available
- Allergic reaction due to not checking medical history
- Extracting the wrong tooth
- Iatrogenic damage to adjacent tooth
- Delay in routine referral
- Delay in urgent referral
- Using dirty instruments
- Treating the wrong patient
What can we do to mitigate these incidents?
BAOS Council Members have been involved in the introduction of Correct Site Surgery Policies in several Oral Surgery departments across the country and have conducted original research into Patient Safety in Dentistry and Oral Surgery. Tara Renton recently chaired the LocSSIPs (Local Safety Standards for Invasive Procedures) panel for Dental Extractions at RCS England.
Based on both practical experience and research evidence, the main methods for mitigation of these errors are:
- Learning from mistakes – including investigation and root cause analysis
- Engaging the clinical team when developing Correct Site Surgery Policies
- Utilising the LocSSIPs template and guidelines from NHS England/RCS England
- Developing a Correct Site Surgery checklist that is appropriate for your clinical environment
- Providing training for staff on the use of the Checklist
- Ensuring that the Checklist is being used correctly through active audits of the processes involved
- Supporting the clinical team throughout the process and not taking punitive action when incidents do occur
- Develop a positive patient safety culture in your workplace
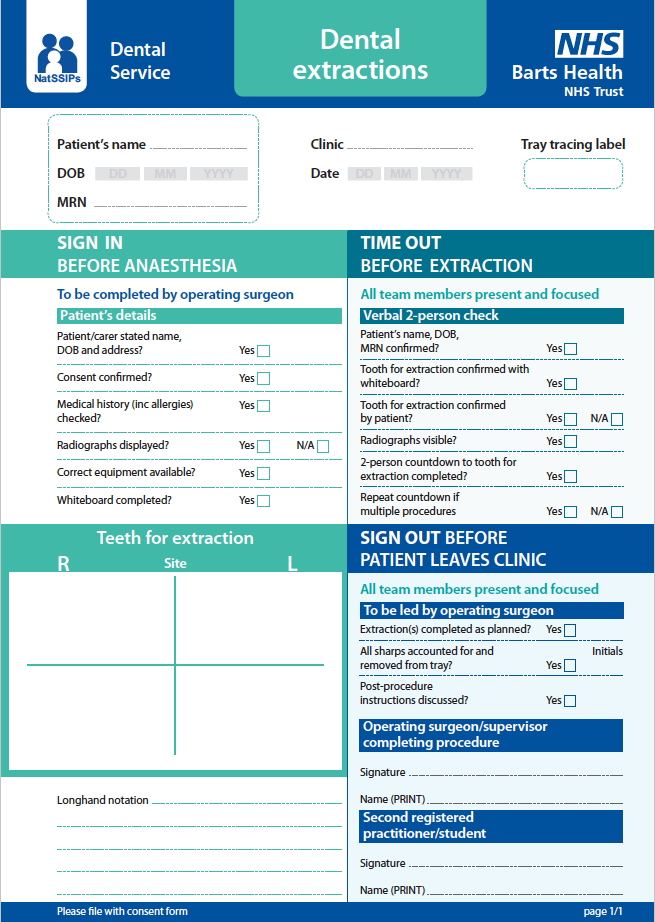
Correct Site Surgery Checklists must incorporate the following stages:
Sign in:
The clinical team check that the correct patient is present and that all of the necessary clinical information and equipment is available and functioning.
Time out:
At this point, the clinical team pause in order to run through the checks to ensure that the correct treatment is about to take place. The LocSSIPs group decided that this should include a two person check with the assisting clinician or nurse.
Sign out:
The correct procedure is verified and the clinical team discuss any problems encountered and decide how to learn from these for future procedures.
An example of a checklist in use at a major London trust is shown below:
Edmund Bailey (2017)
Building a positive patient safety culture

Further information and relevant information
- Sign up to safety pledge
- NHS Never Events Policy
- Tara Renton’s summary presentation on Patient Safety
- Tara Renton’s paper on reporting patient safety incidents (need BDJ access): http://www.nature.com/bdj/journal/v221/n2/full/sj.bdj.2016.526.html
- LocSSIPs pathway for dental extractions – RCS England and NHS England.
- Systematic review of patient safety interventions in dentistry – (open access): https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-015-0136-1
- GDPs views on patient safety (need BDJ access): http://www.nature.com/bdj/journal/v219/n11/full/sj.bdj.2015.920.html
- Patient safety in primary care dentistry (need BDJ access): http://www.nature.com/bdj/journal/v217/n7/full/sj.bdj.2014.857.html
- Link to WHO website http://www.who.int/patientsafety/en/
- Link to NHS England: https://improvement.nhs.uk/resources/examples-local-safety-standards-invasive-procedures/
- https://www.fgdp.org.uk/news/wrong-site-tooth-extraction-removed-never-events-list
- https://www.nature.com/articles/sj.bdj.2017.456
The BAOS has developed a ‘sign up to safety’ pledge with NHS England – the document is available to view by clicking below: